Survivorship
Survivorship
What Is Survivorship?
Anyone who has been diagnosed with cancer—from the moment of diagnosis through the rest of their life is considered a cancer survivor.1 This definition of survivorship shifts the image of a person with cancer from being a ‘victim’ to that of someone who is living with strength and resilience.2 It reinforces an important truth—you are not defined by your diagnosis—you are recognized for your courage, your journey, and the life you continue to lead.
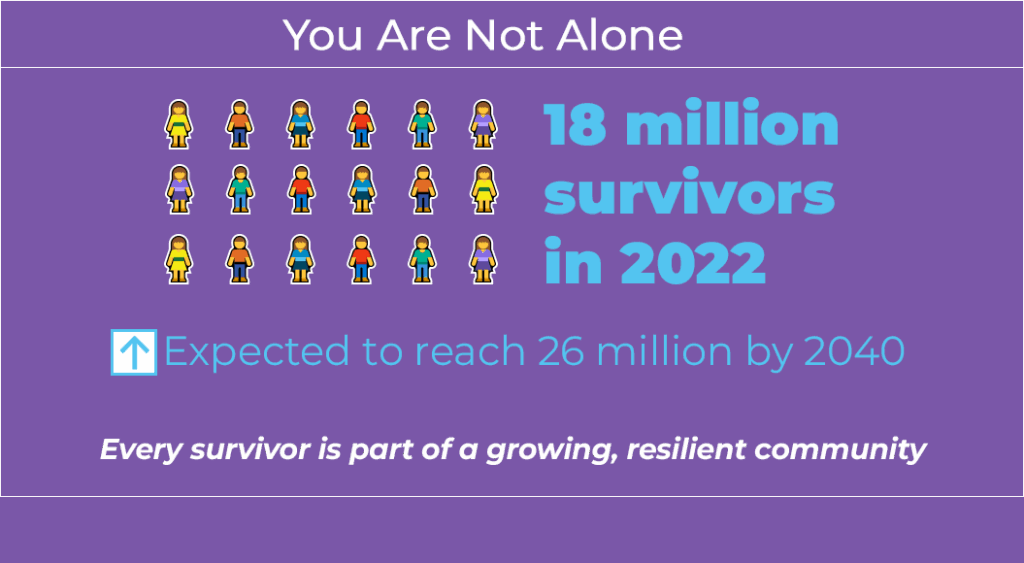
As a cancer survivor, it’s also important to remember that you are not alone! In 2022, there were nearly 18 million cancer survivors in the United States, with that number expected to grow to 26 million by 2040.3 You are part of a large, vibrant, and growing community of people who have faced cancer.4
What Is a Survivorship Care Plan?
Survivorship care is complicated, with many different parts that focus on improving health, wellness, and quality of life while also managing the effects of cancer and cancer treatment. 4 Experts recommend that every survivor receive a written survivorship care plan. This plan should include a summary of your cancer treatment, a schedule for follow-up care, information about possible long-term and late effects, and guidance for healthy living. These documents are created just for you and should be reviewed and updated regularly to match your changing needs.5
Survivorship care plans are meant to ensure that you receive complete follow-up medical care after diagnosis, including:6
- A schedule for routine monitoring and follow-up care that is specific for your cancer
- Watching for signs of new cancers or your original cancer coming back
- Support for physical, psychological, and emotional aspects of your disease and treatment
- Making sure your doctors and healthcare team stay connected and work together
In most cases, your primary care provider will work with your oncologist to determine your needs for ongoing care, starting either during your treatment or after your treatment has finished.4 Nurses and patient navigators also play an important role by focusing on your specific needs, coordinating referrals for services and specialists, and providing you with education and resources. Patient navigators can help with transportation and insurance questions, which often continue after treatment is completed.2
- For more information on the cancer care team, please visit: https://patient.encompass-cancer.com/patient-toolkit/the-cancer-care-team/
Living with the Effects of Cancer and Treatment
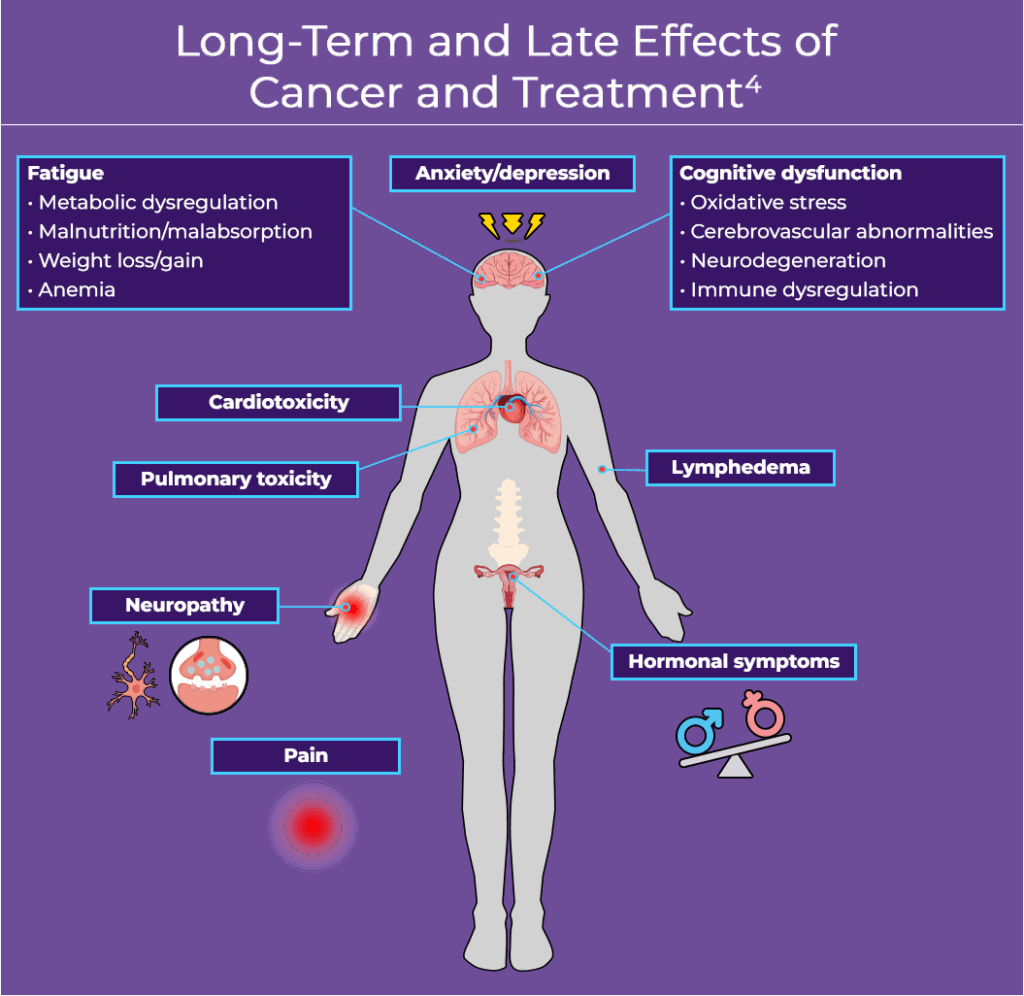
Although many side effects, such as nausea and vomiting, end quickly after treatment, some people experience “long-term effects” which can begin during treatment and last after treatment is finished. Examples of long-term effects are trouble concentrating and fatigue. “Late effects” may start long after treatment has finished, for example, developing a second cancer.4
Cancer and its treatment can have many different effects, and each person may experience them differently. Many survivors experience complications, such as fatigue, pain, and depression.4,7 You may experience some of the conditions listed below, but how and when they occur may be different for you compared to others.
Second cancers: Some people who’ve had cancer may develop a new, different type of cancer, because of certain treatments, risk factors, or conditions that run in families. If needed, your care team may recommend extra tests in addition to routine cancer screenings. In some cases, lifestyle changes, vaccines, or medications can help reduce the risk of a second cancer forming.4
Anxiety, distress, depression and fear of recurrence: Emotional distress is reported by survivors during every stage of their cancer. As many as 45% of patients experience significant distress. In fact, anxiety and depression are the most common mental health problems after a cancer diagnosis. It’s normal to feel a range of emotions during cancer treatment or when there are changes in your disease. These emotional changes can affect your well-being and quality of life. Therefore, routine mental health screening is recommended throughout the cancer journey.7
- For more information on mental health in survivorship care, please visit Staying Mentally Healthy.
Hormonal changes: Cancer treatment can affect your hormone levels, which can cause mild-to-severe hot flashes, mood changes, or other sexual health problems. If you develop hormone-related symptoms, you may benefit from hormone therapy or non-hormonal medications and healthy lifestyle changes.4
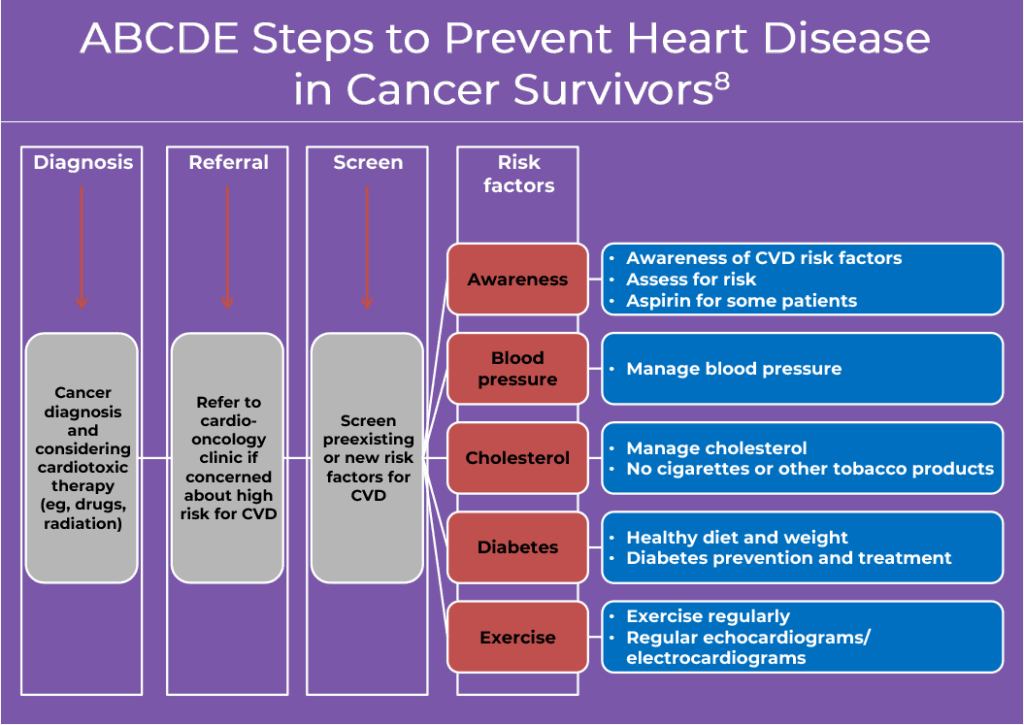
Heart disease: Certain chemotherapy drugs or radiation to your brain, neck, and chest, can damage your heart over time. For this reason, you may be referred to a cardio-oncologist before treatment starts and may also require regular monitoring or lifestyle changes to protect your heart. Staying active, eating a heart-healthy diet, and managing blood pressure or cholesterol can help lower your risk of heart disease. Inform your care team if you develop shortness of breath or chest discomfort. Following the ABCDE tool is recommended for survivors of breast, prostate and other cancers to determine which treatment increases the chance of cardiovascular disease (CVD).4,8
Lymphedema: Lymphedema is a buildup of lymph fluid under the skin, often causing swelling in an arm or leg. It can be short-term or long-lasting after surgery or radiation to your lymph nodes. Lymphedema can be reversed in early stages, so it is very important to report any swelling, tightness, or heaviness in your arms or legs to your care team. Staying active, using compression garments, and specialized massage can help manage symptoms.4
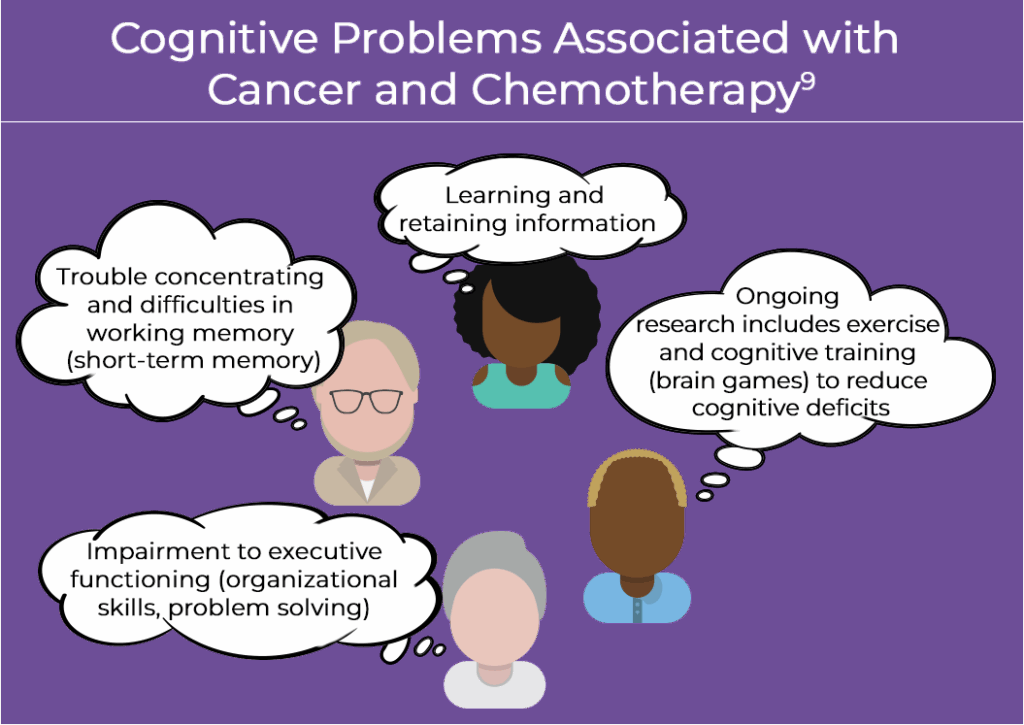
Cognitive dysfunction (brain fog): Many survivors report having changes in their thinking, memory, or ability to focus—often called “chemo brain”. These problems may be caused by cancer itself or by treatments, such as chemotherapy, hormone therapy, radiation, or surgery. If you’re having trouble with memory, attention, or clear thinking, talk to your provider. Support may include education, counseling, or tools to help with your daily routine. The good news is that these changes usually don’t get worse over time. Activities, such as exercise, cognitive training, therapy, and medication can help.4
Sexual dysfunction: Many survivors experience sexual problems due to treatment. Surgery, radiation, and hormone therapies can affect sexual organs, hormone levels, and nerve function. These changes may lower sexual interest, cause discomfort, or affect physical functioning. Let your provider know if you’re having concerns—they can help identify the cause and offer medications, physical therapy, or other options for support.4
Fertility: Cancer and cancer treatment can affect your ability to have children. Ask your care team early on about how your fertility may be impacted by your treatment and discuss any plans for having children. A fertility specialist can explain your options. Some fertility-preserving methods, like sperm banking and egg or embryo freezing, need to be done before treatment begins. Other methods, like shielding or hormone injections, can protect fertility during treatment.4
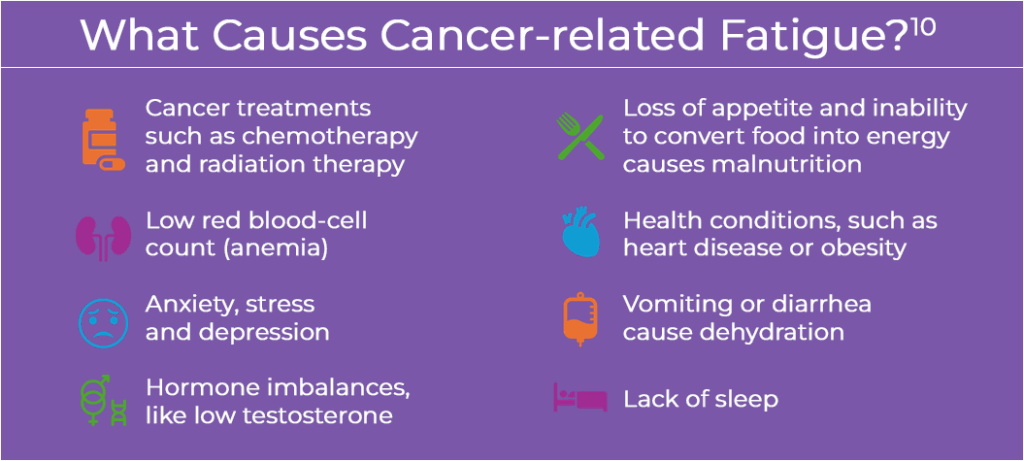
Fatigue: Fatigue is a common and lasting side effect for many survivors. Between 80% and 100% of all patients with cancer experience fatigue beyond what is considered normal tiredness.10 It may be caused by the cancer itself, treatment, sleep problems, or emotional stress. Your provider can help find the cause and suggest ways to manage fatigue, such as exercise, sleep support, counseling, or medications.4
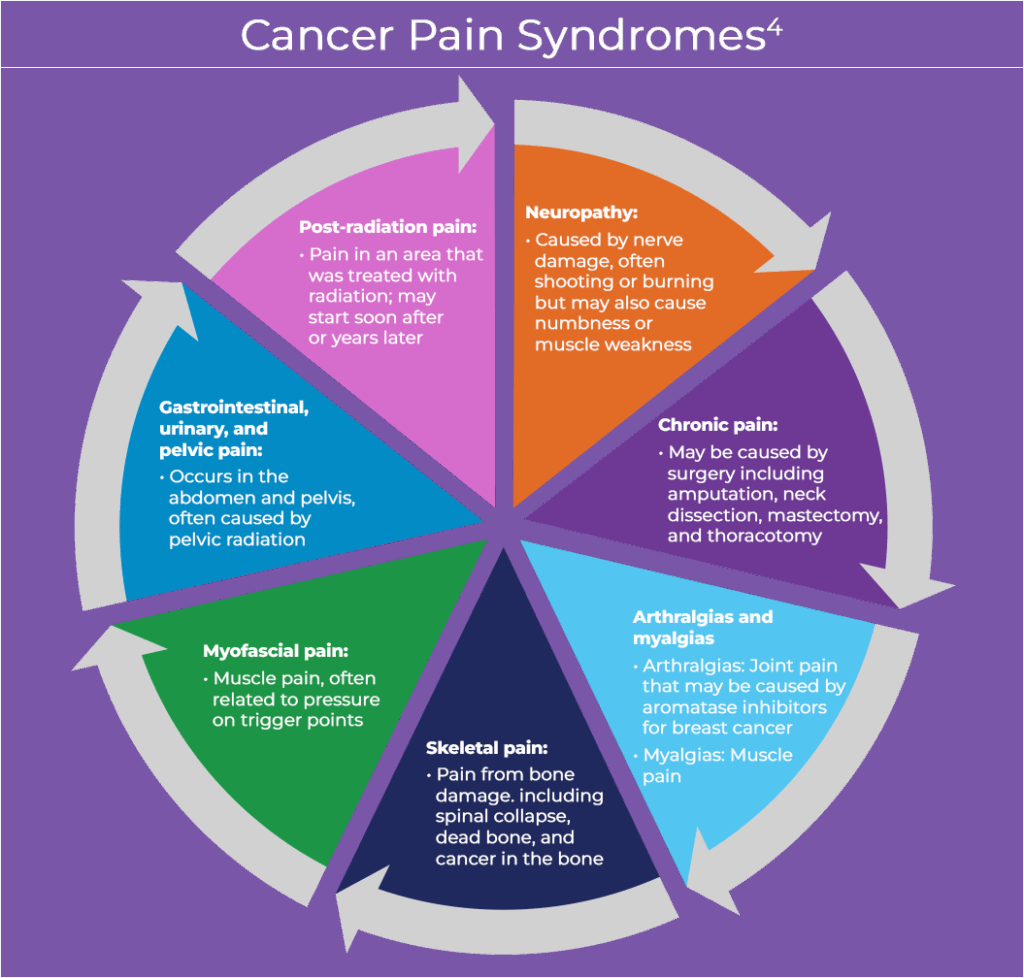
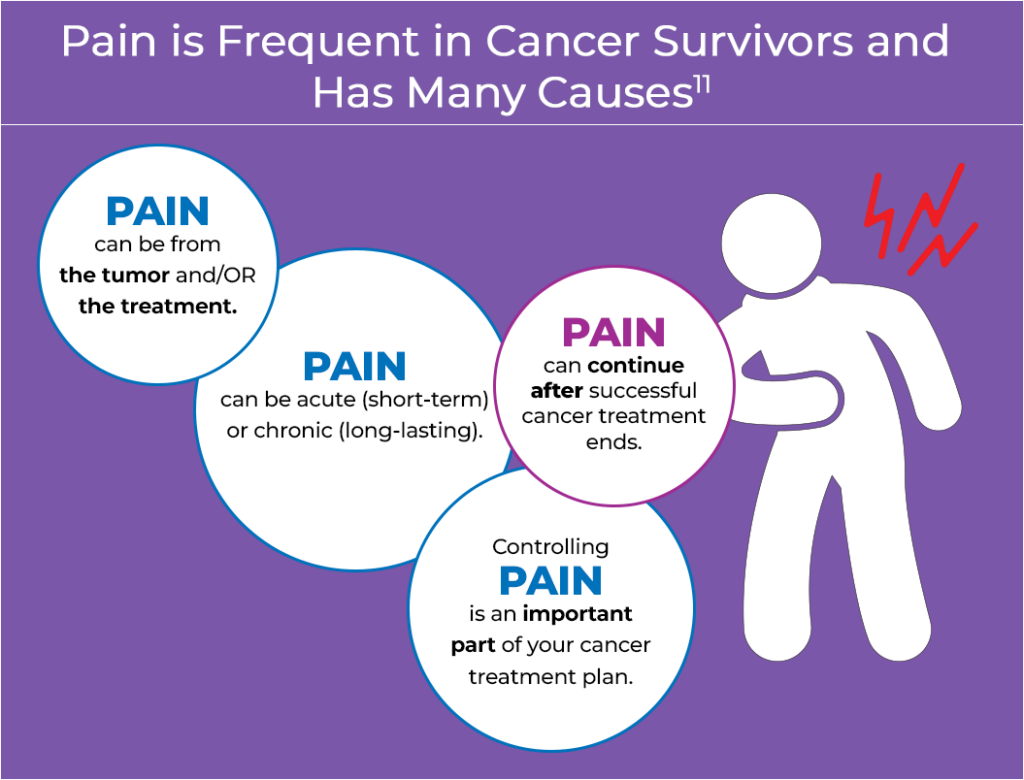
Pain: Pain in cancer survivors, including pain syndromes, is common and has a wide array of causes. In fact, more than 1 in 3 survivors have chronic pain.4,11 Common types of pain experienced by cancer survivors are shown in the figure below.4
Pain assessments are a part of routine oncology care and may include brief pain screenings, detailed pain evaluations, and referral for pain management depending on the unique needs for each patient. Many classes of medications (eg, oral, topical) are used in managing pain, as are non-drug options, such as physical therapy. Mental health and alternative approaches are also used, such as cognitive behavioral therapy, acupuncture, or mind and body treatment.4 Fortunately, the Centers for Disease Control and Prevention has put together guidelines and education for healthcare providers to help ensure the safe use of opioid medications for patients who need them as part of a multi-pronged approach to manage chronic pain.12
- For more information on side effects of cancer treatment, please visit: https://patient.encompass-cancer.com/patient-toolkit/understanding-treatment-side-effects/
Living Well After Cancer
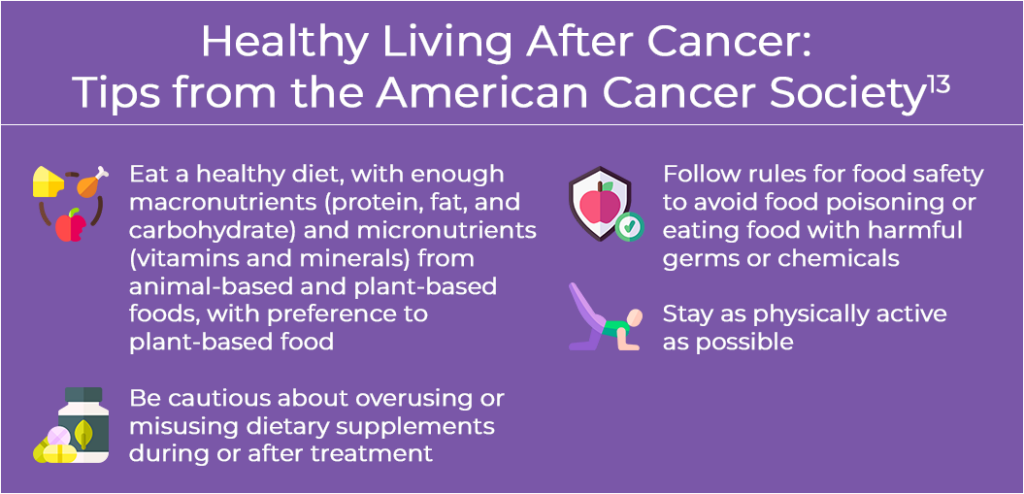
Healthy behaviors, such as quitting smoking, keeping active, and staying at a healthy weight are important during survivorship. In fact, research shows that exercise may improve fatigue and quality of life, as well as helping survivors live longer.13
Eating healthy: Good nutrition is important for everyone, and it’s especially important if you have cancer. As part of your care, you’ll receive information about healthy eating, have your nutrition checked to make sure you’re getting what your body needs, and get a personalized eating plan tailored to your health and treatment goals. Your care team will continue to monitor your nutrition over time. Even though cancer treatments have improved, many people still have trouble getting enough nutrition because of symptoms or side effects, which can affect their health and recovery.13
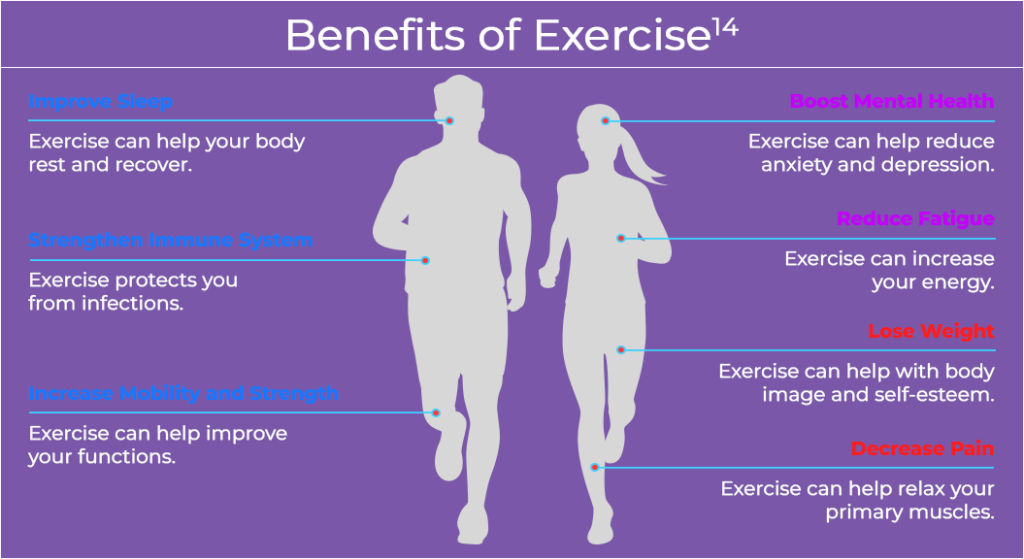
Physical activity: Being physically active leads to positive results even when someone is in pain, including reducing cancer-related symptoms and improving how you feel.14 Physical activity increases strength and your ability to move. Exercise has been shown to improve joint stiffness and pain (called “arthralgia”) which can be caused by certain cancer drugs. However, if you have a fracture or collapse of your spine from weak bones, you may need bed rest before starting any weight-bearing exercises. Physical therapy is often recommended by physicians and is a helpful part of treatment to teach patients how to exercise with less pain. Physical therapy also improves flexibility and strength to increase comfort during routine activities of normal living. Exercising in a pool may also be recommended.4,14
Getting restful sleep: Many survivors have trouble sleeping or have poor sleep quality. Some people have a sleep-wake disorder which makes it hard to fall asleep at night and causes exhaustion during the day. Healthy sleep habits and sleeping for seven to nine hours daily (called “sleep hygiene”), are especially important to help increase the number of hours you sleep and your quality of sleep. If you are experiencing sleep problems, you may be asked to track your sleep patterns or have a sleep study. Cognitive behavioral therapy for insomnia is often recommended and is a preferred treatment for improving sleep. Sleep medications may also be helpful, but they have some risks. You may be given an iron supplement if your iron is low. If you have obstructive sleep apnea, a continuous positive airway pressure (CPAP) machine may be recommended to improve your breathing while you sleep.4
For more information, please visit the Survivorship Resources and Tools for Patients and Caregivers section of Resources and Support Networks
References
- National Cancer Institute Office of Cancer Survivorship. Definitions. https://cancercontrol.cancer.gov/ocs/definitions
- Journal of Oncology Navigation & Survivorship. Transition to Survivorship. https://jons-online.com/issues/2018/july-2018-vol-9-no-7/transition-to-survivorship
- National Cancer Institute Office of Cancer Survivorship. Statistics and Graphs. https://cancercontrol.cancer.gov/ocs/statistics
- National Comprehensive Cancer Network Guidelines for Patients®. Survivorship Care for Cancer-Related Late and Long-Term Effects. 2024. https://www.nccn.org/patients/guidelines/content/PDF/survivorship-crl-patient.pdf
- Hart NH, Nekhlyudov L, Smith TJ, et al. Survivorship care for people affected by advanced or metastatic cancer: MASCC-ASCO standards and practice recommendations. Support Care Cancer.2024;32:313. doi:10.1007/s00520-024-08465-8
- National Cancer Institute. Office of Cancer Survivorship. Models of Survivorship Care. https://cancercontrol.cancer.gov/ocs/special-focus-areas/models-of-survivorship-care
- Lustberg MB, Kuderer NM, Desai A, et al. Mitigating long-term and delayed adverse events associated with cancer treatment: implications for survivorship. Nat Rev Clin Oncol. 2023;20:527-542. doi:10.1038/s41571-023-00776-9
- Mohammed T, Parekh T, Desai A. Cardiovascular risk management in cancer survivors: Are we doing it right? World J Clin Oncol. 2021;12:144-149. doi:10.5306/wjco.v12.i3.144
- Cognitive Problems from Cancer and Chemotherapy. National Cancer Institute. December 10, 2018. https://prevention.cancer.gov/news-and-events/infographics/cognitive-problems-cancer-and-chemotherapy
- How does cancer-related fatigue differ from normal tiredness? City of Hope. March 28, 2023. https://www.cancercenter.com/community/blog/2023/03/difference-between-tiredness-and-fatigue
- Pain Occurs Frequently in Patients with Cancer and Has Many Causes. National Cancer institute. December 10, 2018. https://prevention.cancer.gov/news-and-events/infographics/pain-occurs-frequently-patients-cancer-and-has-many-causes
- Dowell D, Ragan KR, Jones CM, et al. CDC Clinical Practice Guideline for Prescribing Opioids for Pain – United States, 2022. MMWR Recomm Rep. 2022;71:1-95. doi:10.15585/mmwr.rr7103a1
- Rock CL, Thompson CA, Sullivan KR, et al. American Cancer Society nutrition and physical activity guideline for cancer survivors. CA Cancer J Clin. 2022;72:230–262. doi:10.3322/caac.21719
- Your Physical Health. National Cancer Institute. November 21, 2023. https://www.cancer.gov/rare-brain-spine-tumor/living/self-care/physical-health
ALL URLs accessed October 28, 2025